Notification
Please fill in the information below
Urgent
What you should know before undergoing bariatric surgery
In addition to helping you to lose a substantial amount of weight quickly, bariatric surgery can have a significant impact on obesity health problems. However, before we learn together whether surgery is right for you, it is important to understand that bariatric surgery is not for everyone. Surgery is part of the whole obesity treatment process, in addition to internal medicine treatment, psychological treatment and the maintenance of a strictly scientific diet and lifestyle.
When is a person considered obesity?
Obesity is a complex disorder involving an excessive amount of body fat. Obesity isn't just a cosmetic concern but increases your risk of diseases and health problems.
Obesity is diagnosed when your body mass index (BMI) is 30 or higher. Your body mass index is calculated by dividing your weight in kilograms (kg) by your height in meters (m) squared: BMI (kg/m2) = weight / height2.
BMI < 18.5: Underweight.
18.5 ≤ BMI < 25: Healthy weight.
25 ≤ BMI < 30: Overweight.
30 ≤ BMI < 35: Obese (Class I).
35 ≤ BMI < 40: Obese (Class II).
40 ≤ BMI < 50: Morbid obesity (Class III).
BMI ≥ 50: Super obesity (Class IV).
Risk factors for obesity
Obesity usually results from a combination of causes and contributing factors, including:
- Genetics: Your genes may affect the amount of body fat you store, and where that fat is distributed. Genetics may also play a role in how efficiently your body converts food into energy and how your body burns calories during exercise.
- Family lifestyle: Obesity tends to run in families. If one or both of your parents are obese, your risk of being obese is increased. That's because family members tend to share similar eating and activity habits.
- Inactivity: With a sedentary lifestyle, you can easily take in more calories every day than you burn through exercise and routine daily activities. Having medical problems, such as arthritis, can lead to decreased activity, which contributes to weight gain.
- Unhealthy diet: A diet that's high in calories, lacking in fruits and vegetables, full of fast food, and laden with high-calorie beverages and oversized portions contributes to weight gain.
- Food addiction: When the need for food leads someone to desire and pursue it over other reasonable considerations.
- Medical problems: In some people, obesity can be traced to a medical cause, such as Prader-Willi syndrome, Cushing's syndrome and other conditions.
- Certain medications: Some medications can lead to weight gain if you don't compensate through diet or activity. These medications include some antidepressants, anti-seizure medications, diabetes medications, antipsychotic medications, steroids and beta blockers.
- Social and economic issues: Research has linked social and economic factors to obesity. Avoiding obesity is difficult if you don't have safe areas to exercise. Similarly, you may not have been taught healthy ways of cooking, or you may not have money to buy healthier foods. In addition, you're more likely to become obese if you have obese friends or relatives.
- Age:Obesity can occur at any age, even in young children. But as you age, hormonal changes, a decrease in metabolism and a less active lifestyle increase your risk of obesity.
- Pregnancy: During pregnancy, a woman's weight necessarily increases. Some women find this weight difficult to lose after the baby is born. This weight gain may contribute to the development of obesity in women.
- Quitting smoking: Quitting smoking is often associated with weight gain. And for some, it can lead to enough weight gain that the person becomes obese. In the long run, however, quitting smoking is still a greater benefit to your health than continuing to smoke.
- Lack of sleep: Not getting enough sleep or getting too much sleep can cause changes in hormones that increase your appetite.
Why do you need to treat obesity?
Being obese can not only make people feel frustrated or upset about their appearance, more importantly, it can also cause obesity health problems. Individuals with a body mass index over 30 have a higher risk of premature death from all causes compared with those at a normal weight.
Obesity is associated with health risks including: Arthritis, asthma, carpal tunnel syndrome, depression, dematitis, dyslipidemia hypercholesterolemia, reduced effectiveness of oral contraceptives, gall bladder disease, gastro-esophageal reflux disease (GERD), gout, hypertension, infertility, liver disease, migraines, osteoarthritis, polycystic ovarian syndrome, sleep apnea, sleep deprivation, stress urrinary incontinence; or more serious health issues that may lead to the risk of premature death, such as: Cardiovascular disease, diabetes, metabolic syndrome, pseudotumor cerebri, venous stasis disease, etc.
Treatment of obesity
- Diet, Exercise and Behavior Change: This first step is the most rewarding and healthy weight loss option. If you are unable to lose weight and keep it off on your own, you should ask for the supervision of your primary care physician, a dietitian, a psychologist or even a personal trainer.
- Prescription Medications: If you have or are at risk for one of the obesity health problems above and have a body mass index of 27 or more, your doctor may prescribe one of several weight loss medications that most likely fall into one of two FDA-approved categories: Appetite suppressants, and Lipase inhibitors (to reduce the body’s ability to absorb fat).
- Bariatric Surgery: If you have a BMI of 35 or more and have been unsuccessful in your past weight loss attempts, you may be a candidate for weight loss surgery. In addition to helping you to lose a substantial amount of weight quickly, bariatric surgery can have a significant impact on obesity health problems. Despite the positive effect of bariatric surgery on weight and obesity health problems, it is not the right solution for everyone. In addition to preparing for and going through with surgery, big sacrifices must be made in life after weight loss surgery for patients to be successful.
Are you a candidate for surgery?
Bariatric surgery is not for everyone. Even if you fit the minimum bariatric surgery qualifications below, surgery should always be the treatment of last resort:
- A BMI of 40 or more OR a BMI between 30 and 39.9 with a serious obesity-related health problem like diabetes, high blood pressure, sleep apnea, high cholesterol, joint problems, or others.
- At least 80 lbs (36 kg) overweight.
- Between 18 and 75 years old.
- Have a history of failed weight loss attempts.
- Thoroughly understand that the procedure is just a tool; long-term success requires significant diet and lifestyle changes.
Different bariatric surgeries to choose from
There are 4 types of common bariatric surgery to choose from, including:
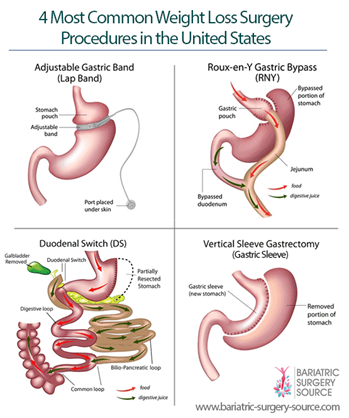
Gastric sleeve (Vertical sleeve gastrectomy) removes about 80% of the stomach, causing patients to feel less hungry and feel full sooner while eating.
Gastric bypass (Roux-en-Y gastric bypass) makes the stomach smaller and reroutes the intestines, causing patients to feel full sooner while eating and absorb fewer minerals.
Lap-band (Laparoscopic adjustable gastric band) wraps an adjustable band around the upper part of the stomach, creating a small stomach pouch above the band that fills up quicker while eating and causes patients to feel full sooner.
Duodenal switch (Biliopancreatic diversion with duodenal switch) makes the stomach smaller, reroutes the intestines, and removes the gallbladder, causing patients to feel less hungry, feel full sooner while eating, and absorb fewer calories and minerals.
There is no “one size fits all” bariatric surgery procedure. Each has its own pros and cons to consider before making a decision:
- Gastric sleeve, gastric bypass, and duodenal switch result in the most weight loss and greatest health improvement but also have longer hospital stays and recovery times and more dietary restrictions.
- LAP-BAND® weight loss is almost as good as sleeve, bypass, and duodenal switch, but it has a lower long-term success rate and requires more follow up visits with your doctor.
These 4 methods are being used in many large obesity centers in the world and at American International Hospital (AIH). In which, Gastric sleeve is the most commonly used, especially for the treatment of diabetes comorbidity obesity.
Efficacy of bariatric surgery
After a bariatric surgery, you can return home in the same day or have a hospital stay of up to 3 days and can be back to work after 3 days to 3 weeks.
You will start losing weight fast after any bariatric surgery procedure, but the total amount lost varies based on the procedure you choose and how closely you follow your doctor’s instructions. For example, depending on your height and weight and chosen procedure, many patients lose up to 100 pounds (45 kg) or more during the first 12 to 18 months after surgery.
Bariatric surgery can help improve the quality of life in 95% of patients and bring 89% reduction in 5-year mortality.
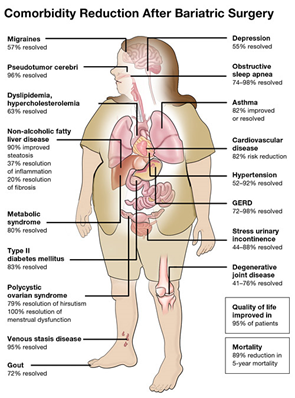
Bariatric surgery may be the best (or only) treatment for those who are morbidly obese. For example, following weight loss surgery, cardiovasscular disease – 82% risk reduction, gastroesophageal reflux disease – 72-98% resolved, migraines – 57% resolved, depression – 55% resolved, pseudotumor cerebri – 96% resolved, obstructive sleep apnea – 74-98% resolved, dyslipidemia hypercholesterolemia – 63% resolved, asthma – 82% resolved, hypertension – 52-92% resolved, metabolic syndrome – 80% resolved, stress urinary incontinence – 44-88% resolved, type II diabetes – 83% resolved, degenerative joint disease – 41-76% resolved, venous stasis disease – 95% resolved, gout – 72% resolved, etc.
Side effects and complications of bariatric surgery
While bariatric surgery carries the same general risks associated with any type of surgery, its safety profile is impressive and its upsides tend to outweigh its risks.
The risk of complications both during and after surgery range from minor to severe. About 10% of bariatric surgery patients have some sort of complication, with the most common being nausea and vomiting. Bariatric surgery has a 99.9% survival rate. About 80% of the deaths that occur within 30 days of surgery are the result of pulmonary embolism, anastomotic leaks or respiratory failure.
Bariatric surgery side effects range from minimal to extensive, depending on the procedure. The most common ones include:
- Digestion issues such as difficulty swallowing, constipation, diarrhea, nausea, or intolerance to certain foods.
- Sagging skin from rapid weight loss.
- Vitamin or mineral deficiency, especially after gastric bypass and duodenal switch.
- Gallstone formation (as a result of rapid weight loss – usually temporary).
- Hair loss (as a result of rapid weight loss – usually temporary)
However, the long-term risks of remaining obese are much greater than the risks of bariatric surgery. Individuals suffering from obesity are 50% more likely to die over any period of time than weight loss surgery patients.
Will you have to change your diet after bariatric surgery?
Pre-Bariatric Surgery Diet: Eating right before surgery will lower your risk of complications and lead to more long-term weight loss. Requirements for each procedure are different, but most pre-bariatric surgery diets include: Healthy food choices, lots of protein, low-carbohydrates, plenty of fluids, certain bariatric vitamins (depending on your lab work results).
Post-Bariatric Surgery Diet: After surgery you will slowly transition from a clear liquid diet to solid foods. Each surgeon is different in their approach, but the typical transition schedule lasts from 4 to 6 weeks. Once you’ve fully transitioned, your new long-term bariatric diet will include:
- Healthy “whole” foods (avoid anything that’s processed).
- High protein.
- Minimal sugar and “simple” carbohydrates.
- Plenty of non-sugary fluids.
- Minimal snacking.
- Smaller portion sizes.
- Slower and more thorough chewing.
- No drinks with meals.
- Strict regimen of bariatric vitamins and supplements.
- Minimal alcohol.
Specific implications for each type of procedure:
- Gastric sleeve patients risk stretching out their smaller stomachs if they overeat, resulting in weight regain. They may also have difficulty swallowing if they eat too fast.
- Gastric bypass patients often cannot tolerate ANY sugar without experiencing unpleasant digestive issues (“dumping syndrome”).
- LAP-BAND patients often experience difficulty swallowing if they try to eat too fast, and they can’t eat or drink anything within 30 minutes of meals.
- Duodenal switch patients have much stricter vitamin regimen to prevent malnutrition, in addition to the same issues as gastric sleeve patients.
Do Minh Hung, MD. PhD.
Head of General Surgery Department, American International Hospital (AIH)
Search
Latest News
Our Doctor






Leave a comment